- by Dr. Leah Deutsch
What is pelvic girdle pain?
Pelvic girdle pain is probably one of the most common things I talk about, both to my students as a pregnancy yoga teacher and as an obstetric doctor. It can be such a debilitating condition and can range from occasional discomfort to debilitating pain and wheelchair bound immobility.
Pelvic Girdle pain can affect both men and women but it predominantly affects pregnant women, with a small group persisting after pregnancy. If you’re pregnant there’s a 20% chance that you may be suffering from symptoms of pelvic girdle pain. If you add in lower back pain to the mix, the numbers are well over 50%, with some studies reporting up to 70%. Basically it’s really common!

This condition can start anywhere between 14-30 weeks of pregnancy. You may experience pain in the sacro-iliac joints at the inner aspect of your buttocks, which may radiate across the whole buttocks or into your thigh. Some people may also experience a pain at the front of the pelvis over the pubic bone. It’s really important to say that your healthcare provider should check for possible red-flag symptoms like fever, neurological impairment or lumbar spine or disc issues, to exclude anything more serious, before giving this diagnosis.
Understanding the structure of the pelvis and what happens to the body in pregnancy is a real key to gaining an empowered awareness of what’s happening in this condition.
Breaking Down the Anatomy and Physiology
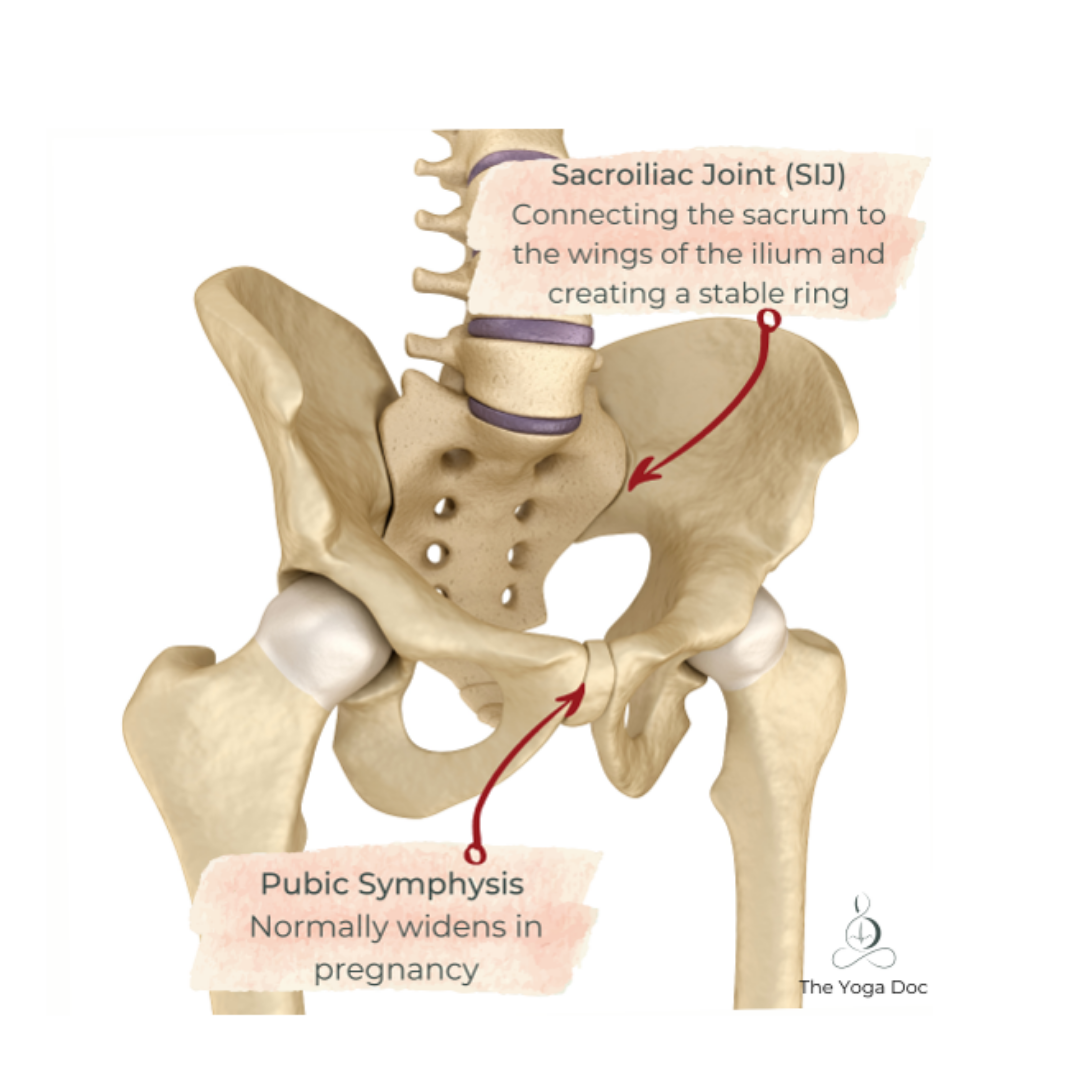
The pelvis is a really solid and strong structure. It’s made up of 3 bones, the sacrum a fused part of your spine, which is like a solid plate sitting at the base of your spine, between your lumbar spine and your coccyx and the two wing like structures of the pelvis, the ilium, which connect to the sacrum at the back of your pelvis and are fused together at the front, to form your pubic symphysis. This creates a really strong and stable ring or bowl like structure. The stability of this joint is a really key point to remember, which we’ll revisit later.
In pregnancy the production of several hormones (predominantly relaxin), causes a relaxation of the ligaments throughout the body. This is a normal and natural process of pregnancy, which all women will go through. Unfortunately this fact has led to a now widely regarded false theory, which attributes this normal laxity to the cause of pelvic girdle pain. Spoiler, it’s not!
Debunking Healthcare Myths
This biomechanical model, which is often used as an explanation to those suffering by well meaning healthcare and exercise industry professionals alike, sadly worsens the problem, by feeding in to fear based beliefs from those who we put our trust in and go to for help.
Studies have in fact shown the biomechanical theory to be false. Although relaxin is responsible for a shift in pelvic anatomy, there is little to no correlation between levels of relaxin and symptoms of PGP (see systematic review in references). Other studies have shown that the natural widening in the gap at the front of the pelvis (the pubic symphysis) increases gradually through pregnancy and wider gaps are associated with those presenting with more severe PGP, but it’s important to say there’s no linear correlation.
This is where I have to hold my hands up to say that I myself have in the past perpetuated this myth, having had it passed down to me through the medical education system, which shows how widely spread it is. My understanding has completely shifted in recent years, through exploring the research and educating myself with evidence based sources on this topic.
Studies have consistently shown that the factors which increase the chance of suffering from this condition are:
• Prior history of pregnancy
• Smoking
• Joint hypermobility
• Pelvic floor dysfunction
• A raised BMI
• A history of trauma or lower back pain
• Work dissatisfaction
• A lack of belief in improvement

Reframing the Conversation
The biopsychosocial model for understanding pain is really interesting and is deeply rooted in our psyche as humans. The logical impulse that tells us that pain means that there’s something wrong, is an important and protective mechanism. It alerts us to remove a hand from a hot surface, or lift our foot, when we step on something sharp, due to the pain fibres being activated, but did you know that pain fibres or noccipetors can be activated without a physical stimulus and aren’t always a sign that harm is being done.
When we believe that pain equals harm and these views are reinforced by trusted healthcare providers telling us that something is out of place, misaligned or ‘unstable’, it feeds in to this already strongly held belief and contributes to fear of moving our bodies, due to the falsely held notion that our pelvis’ are vulnerable structures.
We consequently adopt strategies of movement restriction or avoidance with muscle tensing or guarding, but in fact, we know that these strategies can actually worsen pain symptoms. When we brace or guard against movement, it loads the tissues more and potentially can worsen the pain experience, further fuelling this fear-avoidance cycle.
I think it’s really important at this point, to say this is not all in the mind or de-legitimise the experience of pain. As doctors we often seek for a bio-medical explanation to explain a symptom and the complexity of this relationship can mean the person suffering feels stigmatised if a physical cause is not found. This is why the importance of understanding the multi-factorial contributors to pelvic girdle pain is so important.
We know that when pelvic girdle pain becomes disabling it’s not a feature of the pelvic bones becoming unstable or out of place, it’s in fact the structures (tissue) around the pelvis becoming highly sensitised. The evidence we have tells us that tissue sensitivity is a predictor of how bad PGP is and is directly related to high levels of stress, lack of sleep, altered body position and coping with the complex interactions of relationship changes and new roles in pregnancy. This all acts to wind up the nervous system at a vulnerable time, further perpetuating fear. I’ll say it again, if we can understand the mechanism it can help reduce the fear and help with symptoms.
How to Help
The key to managing this painful condition, is seeking help early, identification and adopting strategies of:
- Functional integration
- Graded exposure
- Overcoming avoidance
1. Physiotherapy
Seek out a women’s health physiotherapist, who is used to supporting women with this condition. By getting early intervention and being supported with a combination of education and movement strategies, you can really improve your outcomes.

2. Exercise
Exercise has been shown to help with symptoms in multiple studies. I always reiterate how it’s so important to listen to your body and work within your own parameters, but we know that in those who took part in activity, studies consistently show that symptoms improve. I may be biased, but yoga is a really fantastic tool in alignment based gentle movement to help overcome avoidance, check out my completely free Pregnancy Yoga videos for more. (www.YouTube.com/c/TheYogaDoc)

3. Pregnancy Support Belt
Pelvic girdle belts support bands have mixed evidence in terms of helping, but this can help and has been shown to cause no harm in pregnancy. The only proviso here is to remember that this can reinforce the perception that your pelvis is somehow unstable and needs ‘support’, which as we’ve established it does not. Many women do find these helpful though, so it may be something you wish to try.

4. Pregnancy Support Pillows
The recommended advice is to sleep on your left side from 24 weeks and with a growing bump, this position can become uncomfortable and being in this fixed tilted position for long periods, can increase symptoms of discomfort at night, leading to lack of sleep. As we’ve already established, lack of sleep contributes heavily to symptoms of pelvic girdle pain, so using a pregnancy support pillow such as the BellaMoon 3-in-1 can be hugely beneficial in helping your symptoms.
5. Mindset
Finally, one of the strongest predictors in those doing better are those who believe they will do better, just read that again. Incredibly the health belief that things will get better, is correlated to symptoms improving. So trying to give people good coping strategies to keep active and relaxed and adjust body positions to help prevent the wind up of the nervous system is key here. Building confidence and understanding of the mechanisms and using strategies to move normally and trust your body is so important in helping.

For more pregnancy related support from Dr Leah Deutsch check out her websites:
https://www.thebirthcollective.org/
Youtube Channel - https://www.youtube.com/channel/The-Yoga-Doc
Or follow her on Instagram @yoga_doc
References
- Pelvic Girdle Pain in the Antepartum Population: Physical Therapy Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health From the Section on Women’s Health and the Orthopaedic Section of the American Physical Therapy Association, Clinton SC, (2017), Vol 41, Issue 2, pp102-125
https://journals.lww.com/jwhpt/Fulltext/2017/05000/Pelvic_Girdle_Pain_in_the_Antepartum_Population_.7.aspx
- Understanding and managing pelvic girdle pain from a person-centred biopsychosocial perspective, Beales D, et al; Musculoskeletal Science and Practice 2020; 48
https://doi.org/10.1016/j.msksp.2020.102152
- Pregnancy-related pelvic girdle pain and its relationship with relaxin levels during pregnancy: a systematic review, Aldabe D, Eur Spine Journal (2012);21 pp1769-1776
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3459115/
- The adult human pubic symphysis: a systematic review, Becker I, Journal of Anatomy 2010, 217 pp475-487
https://doi.org/10.1111/j.1469-7580.2010.01300.x
- Interview with Professor Peter O’Sullivan, Muscluloskeletal Physiotherapist, Youtube video
https://www.youtube.com/watch?v=HK7SiQtyqxw
Dr Leah Deutsch has extensive experience supporting women through their fertility journey in to pregnancy, birth and beyond as an NHS doctor in obstetrics & gynaecology. She works as a senior registrar in a busy London hospital and is a member of the Royal College of Obstetricians & Gynaecologists.

As if that isn't impressive enough, after discovering the hugely therapeutic practice of yoga for herself in 2001, Leah is now also a practising Yoga Alliance registered teacher, having trained internationally with a number of highly regarded teachers and holding advanced 500+ hour trainings in Vinyasa, Ashtanga, Hatha, Yin and pregnancy yoga, influencing her teaching style and helping facilitate balanced and intelligently sequenced classes. She now has a dedicated Instagram community under the name @yoga_doc where she provides fantastic resources, advice and support on all things fertility, pregnancy and postpartum.
We caught up with Dr Leah to find out more about the bothersome pregnancy symptom, Pelvic Girdle Pain; why exactly we suffer from it and ways we can reduce the pain.

